Why every workplace needs a mental health policy
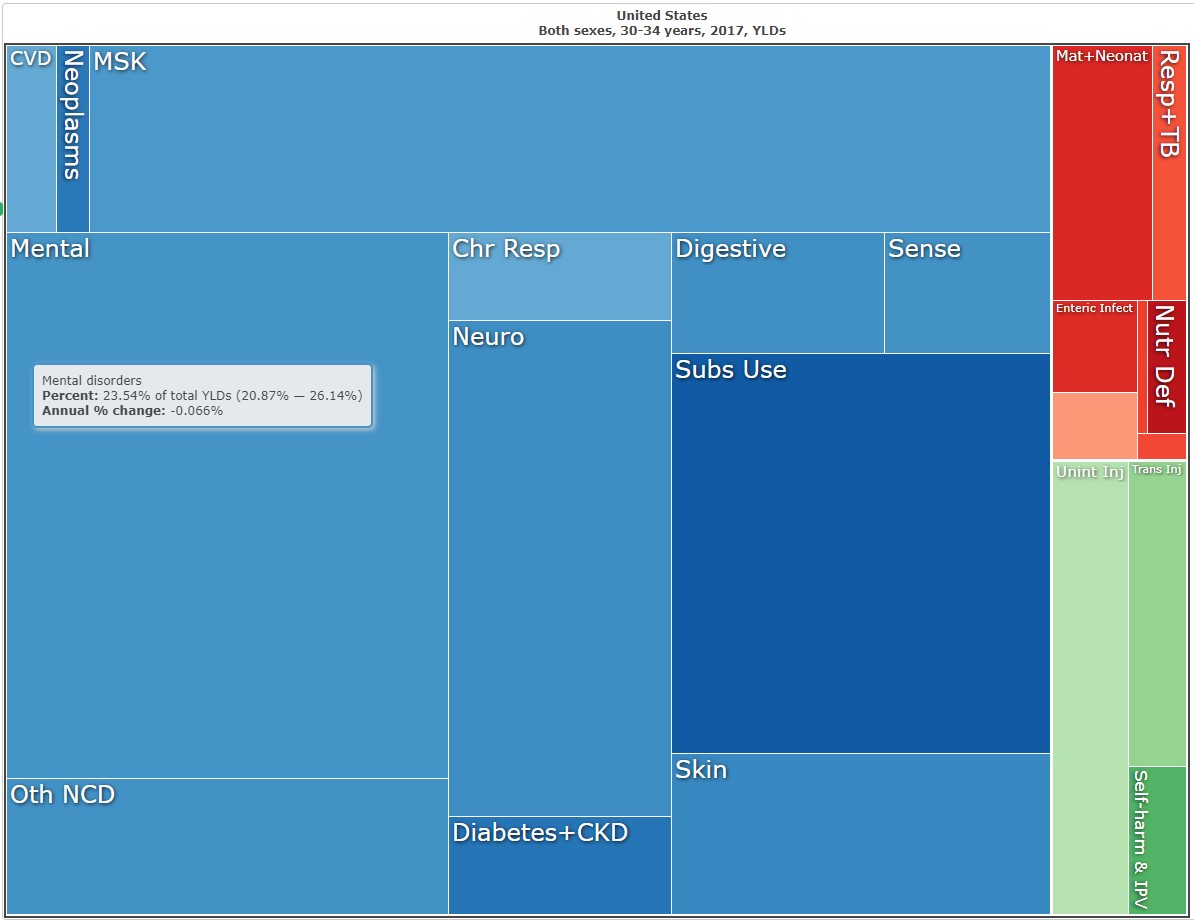
There’s no doubt that mental health is a major burden on the American workforce. In 2017, mental health was the second largest cause of disability among working-age Americans according to the Global Burden of Disease Study1. The burden of mental health disorders is largely driven by persistent depressive disorder, major depressive disorder, and anxiety disorder. To put this in perspective, these estimates suggest that for a company our size (35 employees), and average age (30-35 years), 2.4 employees each year will have a new incident of anxiety or depression, while 5.1 employees have existing (prevalent) cases. This makes for significant impact on the health of our teams.
According to a study in the Journal of American Medicine Association, workers who self-report depression have a significantly higher loss in productive time due to personal health or family reasons compared to those without (5.6 hours per week vs 1.5 hours per week, respectively)2. Therefore, any workplace policy for accommodating personal health or family emergencies would miss the target if it didn’t address the needs of those with depression and/or anxiety. Ideas to remove personal and social stigmas around mental health can dissolve barriers to seeking effective treatment, and this can have meaningful economic impact.
“US workers with depression employed in the previous week cost employers an estimated $44 billion per year in lost productive time, an excess of $31 billion per year compared to peers without depression.”2 It’s in employer’s best interest to accommodate a swift recovery, since early intervention can considerably reduce the duration of an episode.
So what does the employer need to know? The median duration of a new major depressive episode is roughly 12 weeks3 and can extend multiple years in cases that are co-morbid with persistent depressive disorder. Ensuring that the employee gets immediate and stable treatment can have a large impact on their well-being for the duration of that time. So how do we put these pieces together to create a mental health policy?
At Campfire we turned a big win for mental health into a permanent benefit at the company.
Through the work of the Diversity & Inclusion Forum, we discussed and identified the potential impact of de-stigmatizing mental health in the workplace. An employee’s story of the swift and careful accommodation from their project lead became a roadmap for us. This team member bravely shared that “the accommodations the company made when I was unwell went a long way to my getting through that time and feeling better.” Building on the success of their experience, we built a guide for our staff that includes these six things:
Our commitment to the mental health of our employees, and immediate short-term accommodation away from work to find professional assistance from the outbreak of an episode.
Direct links and instructions to find in-network mental health providers and expected costs.
Reasonable expectations for the time required to find a psychiatric provider that is both available, and a good fit. We found that this process can take up to several weeks.
A policy outlining the process for leads or board members to approve long-term accommodation with the supply of a doctor’s note. We do this to ensure employees that mental health emergencies are treated equally to all other reasons for medical and family leave.
An outline of employees federal and state rights for sick, FMLA, and short-term disability to provide multiple paths for accommodation.
Lastly, we underscored that sharing a condition is a personal choice, and good leadership respects the private nature of medical and safety matters.
Through the process of building and socializing this plan, we started important conversations around mental health in the workplace that any company could benefit from. At Campfire, we aim to create an atmosphere where workers feel supported, and not stigmatized for mental health needs, and this results in healthier teams.
For questions about this article, please reach out to diegogm@campfireanalytics.com.
References
“The Global Burden of Disease Study 2017” http://ihmeuw.org/4uft (accessed 07/18/2019)↩
Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of Lost Productive Work Time Among US Workers With Depression. JAMA. 2003;289(23):3135–3144. doi:10.1001/jama.289.23.3135. https://jamanetwork.com/journals/jama/article-abstract/196767 (accessed 07/18/2019)↩
Üstün, T., & Kessler, R. (2002). Global burden of depressive disorders: The issue of duration. British Journal of Psychiatry, 181(3), 181-183. doi:10.1192/bjp.181.3.181 https://www.ncbi.nlm.nih.gov/pubmed/12204924 (accessed 07/19/2019)↩